Introduction
As one of the country’s oldest cities, Philadelphia amassed many nicknames. Each name holds its rich history or story about the city. “The City of Brotherly Love,” for example, comes from the literal meaning of Philadelphia in Greek, and “The Birthplace of America” refers to its role in the signing of the Declaration of Independence and Constitution.
A recent addition is “America’s poorest big city.”[1] Philadelphia has consistently had the highest poverty rate of the top ten most populous cities across the United States. In fact, 21.5% of the approximately 1.59 million Philadelphians currently live in poverty. This is nearly double the official poverty rate in the United States, which was 11.1% in 2023. [2]
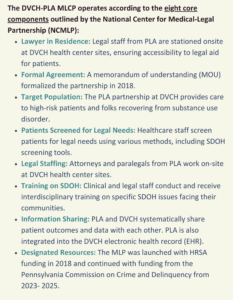
Recognizing the potential for legal services to help healthcare providers respond to social needs seen daily in their clinics, Philadelphia Legal Assistance (PLA) and Delaware Valley Community Health (DVCH) came together to address the barriers to basic needs faced by Philadelphia’s vulnerable communities.
Who They Are: Philadelphia Legal Assistance (PLA) and Delaware Valley Community Health, Inc. (DVCH)
Philadelphia Legal Assistance (PLA) provides free legal services to over 7,000 individuals and families in Philadelphia who cannot afford an attorney annually. They operate several programs, including a Medical Legal Community Partnership (MLCP). “We started this MLP back in 2013 at one City Health Center site in West Philly. Now, we’ve really expanded,” says James Tiderington, Esq., Supervising Attorney in the PLA MLCP.
PLA MLCP partners with Delaware Valley Community Health, Inc. (DVCH), a private, non-profit healthcare organization that operates nine Health Resources and Services Administration (HRSA)-Federally Qualified Health Centers (FQHCs) across Southeastern Pennsylvania. They provide affordable, accessible primary medical, dental, and behavioral health care and preventative services to patients regardless of their ability to pay.
Establishing the Medical Legal Community Partnership (MLCP) at Delaware Valley Community Health
Julia DeJoseph, MD, serves as the Senior Vice President and Chief Medical Officer for Delaware Valley Community Health. She also sees patients at Maria de Los Santos Health Center, a clinic in the Fairhill neighborhood of North Philadelphia that houses one of DVCH’s two MLCPs with PLA.
“I benefit from the [MLCP] resource directly as a provider with my patients. But I also was part of the team that began the partnership,” Dr. DeJoseph says.
A DVCH community board member introduced the organization to the concept of medical-legal community partnerships, emphasizing the importance of support from organizational leadership. “We are really fortunate to have a board member with that type of insight into ways that we could expand care and support for our communities,” Dr. DeJoseph adds.
After getting additional insight into how different programs run their medical-legal partnerships, DVCH determined that partnering with PLA best aligned with their vision for their MLCP.
“We partnered with [PLA] and we met James very early on. We were fortunate that he was the attorney that [we were] linked to. He is a Spanish-speaking individual, and a large percentage of our population are Spanish-speaking, not surprisingly, at Maria de los Santos Health Center. So, it was great to learn about this resource for our patients.”
Dr. DeJoseph views this partnership as a benefit to her patients and fellow providers. As part of her leadership role, Dr. DeJoseph’s goal is to create a wellness model for providers so that they can continue to serve as primary care providers in under-resourced communities for the long term. She views MLCPs as an integrated care model that reduces the burden and responsibility on providers by linking them with legal professionals to address their patients’ non-medical determinants of health.
Keys to Success: Relationship Building, Organizational Integration, and Data
Several key aspects contribute to a successful MLCP, including building a foundation of trust between the medical and legal staff. DVCH and PLA emphasized the importance of integrating the legal staff on-site in the medical setting. “They’re not some external entity. They sit with us in our provider offices at our site. We have group provider offices so that the team is really there. I don’t have my own little, tiny private office that the legal partnership comes to. We are all part of a team,” Dr. Joseph explains.
 This foundation of teamwork and collaboration extends beyond the physical environment to all aspects of the MLCP operations at DVCH. “I think, being on-site, being right there integrated – inviting the medical-legal team to our parties, our theme days, and including them in all of those things – is essential because they truly are part of our team,” Dr. Dejoseph explains. “They’re in our electronic health record (EHR); they’re in our Teams messaging. They’re just the same as we are, even though they work for a different organization.”
This foundation of teamwork and collaboration extends beyond the physical environment to all aspects of the MLCP operations at DVCH. “I think, being on-site, being right there integrated – inviting the medical-legal team to our parties, our theme days, and including them in all of those things – is essential because they truly are part of our team,” Dr. Dejoseph explains. “They’re in our electronic health record (EHR); they’re in our Teams messaging. They’re just the same as we are, even though they work for a different organization.”
Margaret Robinson, Esq., Supervising Attorney in the PLA MLCP, echoes Dr. DeJoseph on the importance of developing strong connections between medical-legal staff for successful MLCPs:
“Integrating into health centers and developing relationships with staff have been really important for our success for not only doing the work, but also for the health centers to see the results of the work. We’ve been able to have access to the EHR at most of our sites and record client patient outcomes in the EHR, which I think has been a contributor to our success to have providers be able to see the results of our work.”
Sometimes EHR integration causes trepidation for organizations on both sides of the medical-legal partnership. James Tidderington, Esq. explains why this is something that should be embraced, when possible, rather than feared:
“I think that we’re really well integrated is what also makes us quite successful. I know there’s other MLPs that are a little bit weary about maybe getting into the EHRs because of Health Insurance Portability and Accountability Act (HIPAA) concerns or they don’t necessarily report back to the provider as to the outcome of the case. They say, ‘Well, just you should go follow up with your patient rather than follow up with me.’ I think the [EHR access] lends to just getting to know the providers and what the needs are at that particular health center. Being more collaborative and integrative are things I think make a really good MLP in the end.”
“Not only does being able to be in the chart make it easier to make the referral and make it simpler, but it reduces some of the risk of exposing information,” Robinson adds.
Leadership for both organizations prioritized formally quantifying the positive financial and social impact of the MLCPs. In addition to tracking case metrics internally, PLA conducted a return on investment study led by private consultant Erin Davison on their MLCPs. This study found that investments in the MLCP between 2018 and 2023 yielded an $11 return for every $1 invested. [3]
These data proved useful in pursuing additional partnerships and funding opportunities:
“James does a really great job on the finances of how much money is saved universally,” says Dr. DeJoseph. “A few years ago, I actually had James and [another DVCHC director] present at [a conference]. While they presented, one of our largest Medicaid payers was in the audience. They fund [MLCPs] now because of that presentation.”[3]
Looking to the Future
DVCH and PLA are working to strengthen and sustain their current capacity while also planning for future growth. Tiderington hopes to prioritize collaboration with MLCPs across the country to build from one another. “I still quote a presentation someone did from the last national meeting in 2019,” he said. “We hope others will sort of see our model and be like, ‘Oh, we can do it, too.’ Let’s continue to build.”
For their part, DVCH is in its first year of operating as the Sponsoring Institution for a family medicine residency program. This program allows the next generation of providers to become familiar with MLCPs early in their medical education.
When asked what helps make a successful MLCP from the health center perspective, Dr. DeJoseph said, “I think in any situation you need a clinical champion. You need somebody who’s going to be able to buy in and truly understand. It generally needs to be somebody in leadership.”
Dr. DeJoseph has clearly fulfilled this role at DVCH and is working to ensure that her students become the clinical champions of the future.
Endnotes
[3] https://philalegal.org/ROmlcp
Acknowledgements
We would like to express our deepest gratitude to James Tiderington, Esq., and Margaret Robinson, Esq. from Philadelphia Legal Assistance and Julia DeJoseph, MD from Delaware Valley Community Health, Inc. who graciously participated in interviews and provided valuable insights and quotes for this MLP Spotlight. Their firsthand experiences and perspectives have been instrumental in highlighting the impactful work done in their community.
This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an FY24 award to the National Center for Medical-Legal Partnership totaling $550,000 with 0 percent financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov.
About the National Center for Medical-Legal Partnership (NCMLP)
NCMLP’s mission is to help health organizations leverage legal services as a standard part of the way they respond to patients’ social needs. With funding from the Health Resources and Services Administration (HRSA), we provide free technical assistance to health centers, primary care associations, and Health Center-Controlled Networks interested in implementing medical-legal partnership strategies. Learn more about us here and subscribe to the MLP Update, our biweekly newsletter.
